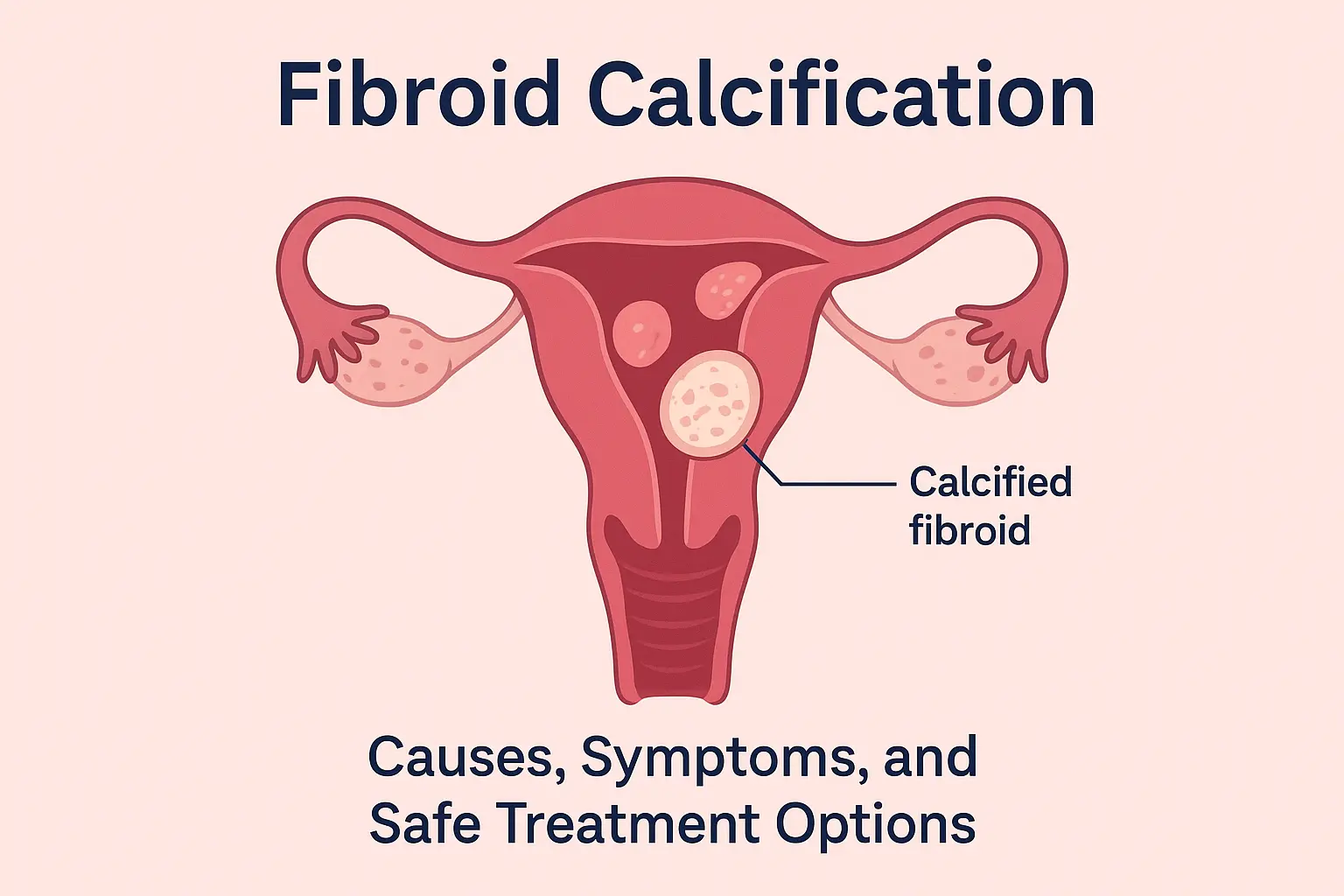
Fibroid Calcification: Causes, Symptoms, and Safe Treatment Options for Women
Fibroids are extremely common among women, especially during the reproductive years. Many women discover them accidentally during scans, while others notice symptoms like heavy periods, pelvic pressure, or stomach bloating. Over time, some fibroids stop growing and begin to harden, a process known as fibroid calcification. Although the word “calcification” may sound alarming, it can actually be a natural part of a fibroid’s lifecycle.
Understanding fibroid calcification is important because many women misunderstand it or worry that it might be cancer. In reality, most calcified fibroids are harmless, but sometimes they can still cause discomfort. With the right information, women can recognize symptoms early, seek timely help, and explore safe gynaecology treatments.
What Is Fibroid Calcification? Understanding Calcified Fibroids
Fibroid calcification happens when a fibroid stops receiving blood supply and begins to shrink. As it shrinks, calcium deposits slowly form inside the fibroid, turning it harder and more solid. This is also known as degenerating fibroid, calcified uterine fibroid, or calcium-deposit fibroid.
Although calcified fibroids are considered non-cancerous, they can still cause symptoms in some women. Understanding this stage helps you recognize whether your fibroid is changing and when to consult a doctor.
Calcified fibroids often occur:
- After menopause
- When a fibroid outgrows its blood supply
- Following pregnancy
- After certain fibroid treatments
Because blood flow reduces naturally with age, fibroid calcification becomes more common in women over 40.
Causes of Fibroid Calcification and Why It Happens
Fibroid calcification usually develops due to reduced blood supply. As the blood flow decreases, the fibroid no longer receives enough oxygen. This leads to a natural process called degeneration, and calcium deposits begin to replace the fibroid tissue.
Common causes include:
- Post-menopausal hormonal changes, which slow blood flow
- Large fibroids, which outgrow their blood supply
- Pregnancy-related changes, as the uterus returns to its normal size
- Previous treatments, such as uterine artery embolization
Because this process happens slowly, many women are unaware of it until symptoms appear or imaging tests reveal calcified fibroids.
Symptoms of Fibroid Calcification That Women Should Watch For
Not all women experience symptoms. However, when calcified fibroids do cause discomfort, the signs are often easier to notice.
Common symptoms include:
- Persistent pelvic pain or pressure
- Lower back pain
- Difficulty emptying the bladder completely
- Constipation due to pressure on the bowel
- Abnormal menstrual changes
- A feeling of heaviness in the lower abdomen
Sometimes the pain improves once the fibroid fully calcifies because the degeneration process is complete. However, if the fibroid is large, pressure symptoms may continue.
If these symptoms begin to affect daily life, it is recommended to speak with a gynaecologist. Early evaluation ensures better and faster treatment options.
How Fibroid Calcification Is Diagnosed in Gynaecology Care
Diagnosis is usually simple and non-invasive. Doctors use imaging tests to understand the size, shape, and calcium levels inside the fibroid.
The most common diagnostic tools include:
- Ultrasound scan, which helps detect calcified areas
- CT scan, used when detailed imaging is needed
- MRI scan, which shows the fibroid’s exact structure
These investigations help doctors decide whether treatment is needed or if regular monitoring is enough. Since calcified fibroids usually grow slowly, they rarely require urgent treatment.
Treatment Options for Fibroid Calcification in Women’s Health
Treatment depends on your age, symptoms, size of the fibroid, and reproductive plans. Many calcified fibroids do not need treatment if they are small and symptom-free.
However, treatment is recommended when symptoms affect daily comfort or quality of life.
1. Observation and Monitoring
Doctors may advise regular scans if the fibroid is stable and painless. This approach is common for women after menopause.
2. Medication for Symptom Relief
Although medicines cannot remove calcified fibroids, they can help with:
- Pain
- Heavy bleeding
- Cramping
Pain relievers and hormonal medicines may be prescribed.
3. Minimally Invasive Procedures
If symptoms persist, minimally invasive options may be used:
- Uterine Artery Embolization (UAE) to reduce blood supply
- Hysteroscopic removal for fibroids inside the uterine cavity
- Laparoscopic surgery for larger fibroids
Because calcified fibroids are harder in texture, doctors choose procedures carefully.
4. Surgical Removal
Surgery is recommended if the fibroid causes severe pressure symptoms or if other treatments do not help.
Types include:
- Myomectomy (fibroid removal while keeping the uterus)
- Hysterectomy (removal of the uterus, usually only for severe cases)
Your gynaecologist will guide you based on your reproductive needs and overall health.
Fibroid Calcification vs Regular Fibroids: What Women Should Know
Understanding the difference helps in choosing the right treatment.
Regular fibroids are soft, whereas calcified fibroids are hard. Because calcification happens after degeneration, symptoms may change.
Key differences:
- Calcified fibroids grow slower
- Pain may reduce after calcification
- Pressure symptoms may continue
- They are easier to detect on scans
- Treatment varies based on hardness and location
Knowing these differences helps women make informed decisions with their doctors.
Practical Tips to Manage Fibroid Calcification Naturally
While lifestyle changes cannot reverse calcification, they can help ease discomfort and improve overall well-being.
- Maintain a balanced diet rich in iron and fiber
- Stay hydrated throughout the day
- Practice gentle exercises, such as walking or yoga
- Use heat pads to relieve pelvic discomfort
- Track symptoms regularly
- Avoid heavy lifting if it increases pain
These habits support your body’s healing process and reduce everyday discomfort.
When to See a Gynaecologist
Seek medical attention if you notice:
- Increasing pelvic pain
- Heavy bleeding
- Bladder or bowel difficulty
- Bloating that does not improve
- Sudden changes in your menstrual cycle
Early treatment not only relieves discomfort but also prevents complications. Since every woman’s body is different, personalized care is essential.
Conclusion
Fibroid calcification is a natural stage that many women experience as part of a fibroid’s lifecycle. Although it may seem worrying at first, it is usually harmless and manageable. By understanding the symptoms, causes, and treatment options, women can feel empowered to take control of their health.
If discomfort persists or daily activities are affected, consulting a gynaecologist is always the safest step. With the right support and guidance, fibroid calcification can be managed effectively, allowing women to return to their normal routines with confidence.
MS.,OG
Gynaecology & Obstetrics
Shifa Hospitals
